Ask the experts: Do you know if you are meeting the Essential Quality Requirements when it comes to decontamination, or what you need to be doing to work towards Best Practice in England? Rachael Painter, practice support consultant at DBG explains.
Firstly, what is the difference between the Essential Quality Requirements and Best Practice?
In the HTM 01-05 it states that if a practice is meeting the Essential Quality Requirements (EQR) the “practices will be expected to provide a statement on plans for future improvement”. On the other hand, for Best Practice (BP) it indicates a practice should reach “the full level of compliance that may be achieved immediately or via a documented improvement from essential quality requirements.”
By using these terms, it identifies the level of compliance a dental practice is meeting.
All dental practices in England must ensure they are meeting the EQR in their decontamination processes. This means all instruments that are reusable must be cleaned using one of these three methods:
Manual cleaning,
Ultrasonic bath or
A washer disinfector.
The instruments should then be visually inspected under an illuminated magnifier before sterilisation. All processes that are used should be validated to ensure instruments have successfully completed each part of the decontamination process.
SO, HOW DO WE ENSURE WE ARE WORKING TOWARDS OR AT BP?
To be able to demonstrate compliance, there are three main areas to focus on:
Firstly - the cleaning process should involve the use of a washer disinfector, ensuring this is being validated.
Secondly - the environment in which the decontamination process in being carried out in should be separate from the area in which you are treating patients.
Thirdly - sterilised instruments should be kept in a separate area to the clinical treatment area to avoid being exposed to aerosols. However, this isn’t always achievable for practices. If you are unable to meet the BP requirements, there needs to be an action plan in place to show your practice is working towards BP and demonstrate you understand what is expected.
The action plan should illustrate what improvements are to be made within your decontamination processes. It should include the following details;
To implement the use of a washer disinfector within your decontamination room.
A plan to create a separate area for the decontamination process away from the clinical treatment area. By separating the cleaning process from the treatment area it will ensure instruments are kept away from potential sources of cross-contamination.
If you have this action plan in place, it will evidence you are working towards BP.
STORING INSTRUMENTS
When it comes to the storage of instruments there is an additional BP requirement: The dental instruments should be stored in an area where cross contamination cannot occur.
The optimal way to achieve this is by storing them in a separate area away from the clinical treatment area. For example, the decontamination room. However, this isn’t necessarily achievable for all practices.
Therefore, to meet the EQR, if instruments are stored in the clinical environment, they must be as far away from the patient chair as possible.
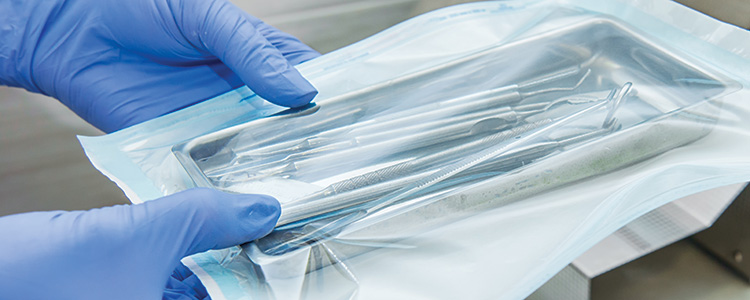
There are alternative methods that can used. Any instrument placed in a pouch pre or post sterilisation, depending on the autoclave type, should be sealed along the perforated edge with the date in which the instruments were placed in the pouch and the initials of the person who carried this out. Instruments in sealed pouches can be stored for up to one year but there must be robust protocols and procedures in place to ensure this is monitored and the date is not exceeded.
Instruments that are in frequent use must remain covered and being stored within the clinical environment must remain covered and protected from aerosols. They can be stored undercover for up to one day but at the end of the working day or the beginning of the next working day, any instruments stored in this way must be reprocessed.
Instruments can also be stored in a non-clinical environment for up to one week providing they remain covered to prevent contamination.
Your use of storage methods should be fully documented and have controls in place to make sure each method used is being robustly monitored and maintained.
If you’d like to develop your knowledge around BP and the EQR we are able to provide practical Infection Prevention and Control Training which is bespoke to your practice.
WE ARE HAPPY TO HELP
If you have any questions why not ask one of our experts to answer tweet us: @THE_DD_UK and use #DDExperts.
For more expert advice contact our dedicated team of training specialists at DD by calling 0800 028 1697 or visiting:
https://www.ddgroup.com/services/training-courses/